Comprehensive Bioinformatics Meta-Analysis of Coronary Artery Disease and Myocardial Infarction
DOI:
https://doi.org/10.58445/rars.67Keywords:
Coronary Artery Disease, Myocardial Infarction, Bioinformatics, Computational BiologyAbstract
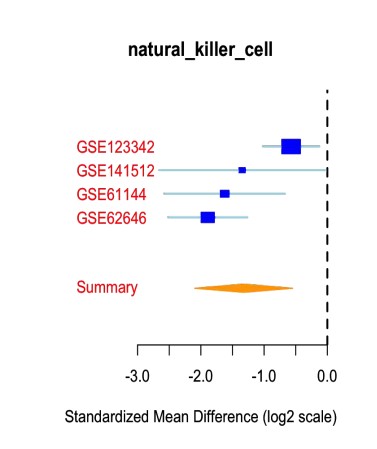
Coronary Artery Disease (CAD) and Myocardial Infarction (MI) are the leading causes of mortality in the United States. Certain genes have been shown through bioinformatics analysis to be related to CAD and MI, but are not incorporated into USPSTF Guidelines. In this study, we aimed to create a model of diagnosis and prognosis in adult patients with coronary artery disease and myocardial infarction from 10 diverse datasets, and also aimed to identify biological pathways, immune cells, and drugs related to CAD and MI to improve biological understanding of these conditions. Using the R MetaIntegrator Package and multiple datasets including the Gene Expression Omnibus, Library of Integrated Network-Based Cellular Signatures, and Reactome, we analyzed data from 10 datasets and found a high predictive value in predicting patients with either CAD or MI. We also used the gene signatures generated through our original meta-analysis to identify significant biological pathways, which included oncogene induced senescence (p < 0.05) and neutrophil degranulation (p = 0.000275), significant drugs that could be potential treatments for CAD or MI, which included enzalutamide (r = -0.5464015, p = 3.043318e-08, FDR = 3.800495e-05) and ibutilide (r = -0.5209267, p = 1.663780e-07, FDR = 9.198588e-05), and significant immune cells using immune cell deconvolution, which included natural killer cells. We conclude that through these results, we have created a more biologically heterogeneous gene signature and meta-analysis to predict diagnosis and prognosis in patients with CAD and MI, and found new biological pathways, drugs, and immune cells that can be used to improve understanding of the conditions and treat them.
References
Brown JC, Gerhardt TE, Kwon E. Risk Factors For Coronary Artery Disease. In: StatPearls. Treasure Island (FL): StatPearls Publishing; June 5, 2021.
Mechanic OJ, Gavin M, Grossman SA. Acute Myocardial Infarction. In: StatPearls. StatPearls Publishing; 2022. Accessed September 22, 2022. http://www.ncbi.nlm.nih.gov/books/NBK459269/
Qi B, Chen JH, Tao L, et al. Integrated Weighted Gene Co-expression Network Analysis Identified That TLR2 and CD40 Are Related to Coronary Artery Disease. Front Genet. 2021;11:613744. Published 2021 Jan 26. doi:10.3389/fgene.2020.613744
Ravi S, Schuck RN, Hilliard E, et al. Clinical Evidence Supports a Protective Role for CXCL5 in Coronary Artery Disease. Am J Pathol. 2017;187(12):2895-2911.
doi:10.1016/j.ajpath.2017.08.006
Coronary artery disease: Causes, symptoms, diagnosis & treatments. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/16898-coronary-artery-disease. Accessed August 11, 2022.
Sweis RN, Jivan A. Acute myocardial infarction (MI) - cardiovascular disorders. Merck Manuals Professional Edition.
https://www.merckmanuals.com/professional/cardiovascular-disorders/coronary-artery-dis ease/acute-myocardial-infarction-mi. Published June 2022. Accessed August 11, 2022.
Hsu J, Smith JD. Genome-wide studies of gene expression relevant to coronary artery disease. Curr Opin Cardiol. 2012 May;27(3):210-3. doi:10.1097/HCO.0b013e3283522198. PMID: 22476029; PMCID: PMC3332306.
Kontou P, Pavlopoulou A, Braliou G, et al. Identification of gene expression profiles in myocardial infarction: a systematic review and meta-analysis. BMC Medical Genomics. 2018;11(1):109. doi:10.1186/s12920-018-0427-x
Geo accession viewer. National Center for Biotechnology Information.
https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi. Published May 5, 2017. Accessed August 2, 2022.
Osmak G, Baulina N, Koshkin P, Favorova O. Collapsing the list of myocardial infarction-related differentially expressed genes into a diagnostic signature. J Transl Med. 2020;18(1):231. doi:10.1186/s12967-020-02400-1
GEO Accession viewer. Accessed September 4, 2022. https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE98583
Nührenberg TG, Langwieser N, Binder H, et al. Transcriptome analysis in patients with progressive coronary artery disease: identification of differential gene expression in peripheral blood. J Cardiovasc Transl Res. 2013;6(1):81-93.
doi:10.1007/s12265-012-9420-5
GEO Accession viewer. Accessed September 4, 2022.
https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE42148
Sinnaeve PR, Donahue MP, Grass P, et al. Gene expression patterns in peripheral blood correlate with the extent of coronary artery disease. PLoS One. 2009;4(9):e7037. doi:10.1371/journal.pone.0007037
GEO Accession viewer. Accessed September 4, 2022.
https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE29111
Vanhaverbeke M, Vausort M, Veltman D, et al. Peripheral Blood RNA Levels of QSOX1 and PLBD1 Are New Independent Predictors of Left Ventricular Dysfunction After Acute Myocardial Infarction. Circ Genom Precis Med. 2019;12(12):e002656.
doi:10.1161/CIRCGEN.119.002656
Veltman D, Wu M, Pokreisz P, et al. Clec4e-Receptor Signaling in Myocardial Repair After Ischemia-Reperfusion Injury. JACC Basic Transl Sci. 2021;6(8):631-646. doi:10.1016/j.jacbts.2021.07.001
GEO Accession viewer. Accessed September 4, 2022. https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE97320
Park HJ, Noh JH, Eun JW, et al. Assessment and diagnostic relevance of novel serum biomarkers for early decision of ST-elevation myocardial infarction. Oncotarget. 2015;6(15):12970-12983. doi:10.18632/oncotarget.4001
Kiliszek M, Burzynska B, Michalak M, et al. Altered gene expression pattern in peripheral blood mononuclear cells in patients with acute myocardial infarction. PLoS One. 2012;7(11):e50054. doi:10.1371/journal.pone.0050054
Valenta Z, Mazura I, Kolár M, et al. Determinants of Excess Genetic Risk of Acute Myocardial Infarction - A Matched Case-control Study. European Journal of Biomedical Informatics. 2012;8(1). doi:10.24105/ejbi.2012.08.1.6
D. Venet, F. Pecasse, C. Maenhaut, H. Bersini, Separation of samples into their constituents using gene expression data , Bioinformatics, Volume 17, Issue suppl_1, June 2001, Pages S279–S287, https://doi.org/10.1093/bioinformatics/17.suppl_1.S279
Haynes WA, Vallania F, Tomczak A, et al. MetaIntegrator: Meta-Analysis of Gene Expression Data. Published online February 26, 2020. Accessed August 13, 2022. https://CRAN.R-project.org/package=MetaIntegrator
Haynes WA, Vallania F, Liu C, et al. Empowering Multi-Cohort Gene Expression Analysis to Increase Reproducibility. Pac Symp Biocomput. 2016;22:144-153.
Khatri P, Roedder S, Kimura N, et al. A common rejection module (CRM) for acute rejection across multiple organs identifies novel therapeutics for organ transplantation. J Exp Med. 2013;210(11):2205-2221. doi:10.1084/jem.20122709
Andres-Terre M, McGuire HM, Pouliot Y, et al. Integrated, Multi-cohort Analysis Identifies Conserved Transcriptional Signatures across Multiple Respiratory Viruses. Immunity. 2015;43(6):1199-1211. doi:10.1016/j.immuni.2015.11.003
Sweeney TE, Braviak L, Tato CM, Khatri P. Genome-wide expression for diagnosis of pulmonary tuberculosis: a multicohort analysis. Lancet Respir Med. 2016;4(3):213-224. doi:10.1016/S2213-2600(16)00048-5
Sweeney TE, Wong HR, Khatri P. Robust classification of bacterial and viral infections via integrated host gene expression diagnostics. Sci Transl Med. 2016;8(346):346ra91. doi:10.1126/scitranslmed.aaf7165
Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society Series B (Methodological). 1995;57(1):289-300.
forwardSearch: Forward Search Function in MetaIntegrator: Meta-Analysis of Gene Expression Data. Accessed September 11, 2022. https://rdrr.io/cran/MetaIntegrator/man/forwardSearch.html
Subramanian A, Narayan R, Corsello SM, et al. A Next Generation Connectivity Map: L1000 Platform and the First 1,000,000 Profiles. Cell. 2017;171(6):1437-1452.e17. doi:10.1016/j.cell.2017.10.049
Vallania F, Tam A, Lofgren S, et al. Leveraging heterogeneity across multiple datasets increases cell-mixture deconvolution accuracy and reduces biological and technical biases. Nat Commun. 2018;9(1):4735. doi:10.1038/s41467-018-07242-6
Khatri P, Sirota M, Butte AJ. Ten Years of Pathway Analysis: Current Approaches and Outstanding Challenges. PLOS Computational Biology. 2012;8(2):e1002375. doi:10.1371/journal.pcbi.1002375
Subramanian A, Tamayo P, Mootha VK, et al. Gene set enrichment analysis: A knowledge-based approach for interpreting genome-wide expression profiles. Proceedings of the National Academy of Sciences. 2005;102(43):15545-15550.
doi:10.1073/pnas.0506580102
Liberzon A, Subramanian A, Pinchback R, Thorvaldsdóttir H, Tamayo P, Mesirov JP. Molecular signatures database (MSigDB) 3.0. Bioinformatics. 2011;27(12):1739-1740. doi:10.1093/bioinformatics/btr260
Fabregat A, Jupe S, Matthews L, et al. The Reactome Pathway Knowledgebase. Nucleic Acids Res. 2018;46(D1):D649-D655. doi:10.1093/nar/gkx1132
Lacy P. Mechanisms of Degranulation in Neutrophils. Allergy Asthma Clin Immunol. 2006;2(3):98-108. doi:10.1186/1710-1492-2-3-98
Zhang N, Aiyasiding X, Li W jing, Liao H han, Tang Q zhu. Neutrophil degranulation and myocardial infarction. Cell Communication and Signaling. 2022;20(1):50. doi:10.1186/s12964-022-00824-4
Chandeck C, Mooi WJ. Oncogene-induced cellular senescence. Adv Anat Pathol. 2010;17(1):42-48. doi:10.1097/PAP.0b013e3181c66f4e
Yan C, Xu Z, Huang W. Cellular Senescence Affects Cardiac Regeneration and Repair in Ischemic Heart Disease. Aging Dis. 2021 Apr 1;12(2):552-569. doi:10.14336/AD.2020.0811. PMID: 33815882; PMCID: PMC7990367.
García-Rivas G, Castillo EC, Gonzalez-Gil AM, Maravillas-Montero JL, Brunck M, Torres-Quintanilla A, Elizondo-Montemayor L, Torre-Amione G. The role of B cells in heart failure and implications for future immunomodulatory treatment strategies. ESC Heart Fail. 2020 Aug;7(4):1387-1399. doi: 10.1002/ehf2.12744. Epub 2020 Jun 13. PMID: 32533765; PMCID: PMC7373901.
Braun NA, Covarrubias R, Major AS. Natural killer T cells and atherosclerosis: form and function meet pathogenesis. J Innate Immun. 2010;2(4):316-24. doi: 10.1159/000296915. Epub 2010 Mar 17. PMID: 20375560; PMCID: PMC2895753.
Sweis RN, Jivan A. Drugs for acute coronary syndromes - cardiovascular disorders. Merck Manuals Professional Edition.
https://www.merckmanuals.com/professional/cardiovascular-disorders/coronary-artery-dis ease/drugs-for-acute-coronary-syndromes. Published June 2022. Accessed August 13, 2022.
Bai L, Scott MKD, Steinberg E, et al. Computational drug repositioning of atorvastatin for ulcerative colitis. Journal of the American Medical Informatics Association. 2021;28(11):2325-2335. doi:10.1093/jamia/ocab165
Mueller HS, Antman EM, Ferst JA, Muller JE. Nifedipine in the treatment of cardiovascular disease. Pharmacotherapy. 1981;1(2):78-94. doi:10.1002/j.1875-9114.1981.tb03555.x
Homans C, Yalcin EB, Tong M, et al. Therapeutic Effects of Myriocin in Experimental Alcohol-Related Neurobehavioral Dysfunction and Frontal Lobe White Matter Biochemical Pathology. JBBS. 2022;12(02):23-42. doi:10.4236/jbbs.2022.122003
Glaros EN, Kim WS, Wu BJ, et al. Inhibition of atherosclerosis by the serine palmitoyl transferase inhibitor myriocin is associated with reduced plasma glycosphingolipid concentration. Biochem Pharmacol. 2007;73(9):1340-1346.
doi:10.1016/j.bcp.2006.12.023
Mullard A. FDA approves first-in-class SYK inhibitor. Nature Reviews Drug Discovery. 2018;17(6):385-385. doi:10.1038/nrd.2018.96
Farooq MZ, Lingamaneni P, Farid S, et al. A Systematic Review and Meta-Analysis of Cardio-Vascular Side Effects with Fostamatinib a Spleen Tyrosine Kinase Inhibitor. Blood. 2019;134:3465. doi:10.1182/blood-2019-132151
Davis ID, Martin AJ, Stockler MR, et al. Enzalutamide with Standard First-Line Therapy in Metastatic Prostate Cancer. New England Journal of Medicine. 2019;381(2):121-131. doi:10.1056/NEJMoa1903835
Kulkarni AA, Rubin N, Tholkes A, et al. Risk for stroke and myocardial infarction with abiraterone versus enzalutamide in metastatic prostate cancer patients. ESMO Open. 2021;6(5):100261. doi:10.1016/j.esmoop.2021.100261
Szymanski MW, Cassagnol M. Ibutilide. In: StatPearls. StatPearls Publishing; 2022. Accessed August 13, 2022. http://www.ncbi.nlm.nih.gov/books/NBK526021/
Das MK, Cheriparambil K, Bedi A, et al. Cardioversion of atrial fibrillation with ibutilide: When is it most effective? Clin Cardiol. 2006;25(9):411-415. doi:10.1002/clc.4960250904
Downloads
Posted
Versions
- 2022-12-20 (6)
- 2022-12-20 (5)
- 2022-12-20 (4)
- 2022-12-20 (3)
- 2022-11-16 (2)
- 2022-11-10 (1)
Categories
License
Copyright (c) 2022 Rachana Gurudu

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.

