Alterations in neuroendocrine levels and gut microbiota contributing to potential psychiatric disorder prevalence in PCOS: a Review
DOI:
https://doi.org/10.58445/rars.57Keywords:
PCOS, Neuroscience, Neuroendocrine, Psychiatry, anxiety, microbiome, gut-brain, microbiota, endocrinology, gynecology, depression, Mental health, Ovaries, Poly Cystic Ovary Syndrome, Poly Cystic Ovarian SyndromeAbstract
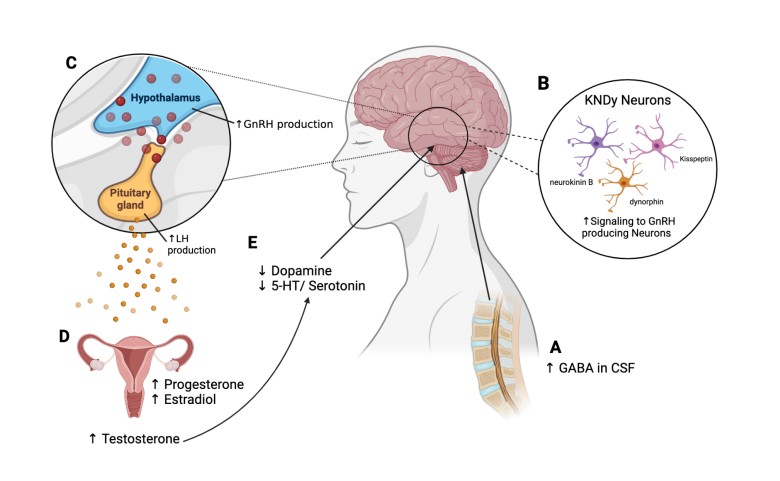
Polycystic ovarian syndrome (PCOS) is the most common endocrine disorder in women, affecting up to 15% of women in the reproductive age. PCOS is a heterogeneous disorder, meaning that there are many different factors that may play a role in the manifestations of this disease, and multiple systems throughout the body can be affected. Studies have shown that PCOS can be linked to multiple psychiatric disorders. The prevalence of anxiety and depression are significantly higher in females with PCOS compared to females without PCOS. Currently, there are several theories discussing the possible causes of the connection between PCOS and psychiatric disorders. Certain causes such as the overactive hypothalamic-pituitary-adrenal axis (HPA axis) or the hypothalamic-pituitary-ovarian axis (HPO axis) found in PCOS could be linked to an altered hormonal profile that manifests as anxiety and depression. Another theory speculates that the altered levels of neurotransmitters and the gut-brain axis dictate the severity and frequency of psychiatric disorders in PCOS. Dietary supplements such as vitamin D and selenium paired with a probiotic have shown to improve neurotransmitter levels as well as significantly reduce the effects of mental distress and manifestations of PCOS symptoms. This approach introduces the possibility of gut nutrient deficiencies in PCOS causing psychiatric disorders. In this review, I will examine different theories on association between PCOS and psychiatric disorders.
References
Almeshari, W. K., Alsubaie, A. K., Alanazi, R. I., Almalki, Y. A., Masud, N., & Mahmoud, S. H. (2021). Depressive and Anxiety Symptom Assessment in Adults with Polycystic Ovarian Syndrome. Depression Research and Treatment, 2021, 1-8. https://doi.org/10.1155/2021/6652133
Alur-Gupta, S., Chemerinski, A., Liu, C., Lipson, J., Allison, K., Sammel, M. D., & Dokras, A. (2019). Body-image distress is increased in women with polycystic ovary syndrome and mediates depression and anxiety. Fertility and Sterility, 112(5), 930-938.e931. https://doi.org/10.1016/j.fertnstert.2019.06.018
Balikci, A., Erdem, M., Keskin, U., Bozkurt Zincir, S., Gulsun, M., Ozcelik, F., . . . Ergun, A. (2014). Depression, Anxiety, and Anger in Patients with Polycystic Ovary Syndrome. Noro Psikiyatri Arsivi, 51(4). https://doi.org/10.5152/npa.2014.6898
Berni, T. R., Morgan, C. L., Berni, E. R., & Rees, D. A. (2018). Polycystic Ovary Syndrome Is Associated With Adverse Mental Health and Neurodevelopmental Outcomes. The Journal of Clinical Endocrinology & Metabolism, 103(6), 2116-2125. https://doi.org/10.1210/jc.2017-02667
Brutocao, C., Zaiem, F., Alsawas, M., Morrow, A. S., Murad, M. H., & Javed, A. (2018). Psychiatric disorders in women with polycystic ovary syndrome: a systematic review and meta-analysis. Endocrine, 62(2), 318-325. https://doi.org/10.1007/s12020-018-1692-3
Chaudhari, A. P., Mazumdar, K., & Mehta, P. D. (2018). Anxiety, Depression, and Quality of Life in Women with Polycystic Ovarian Syndrome. Indian Journal of Psychological Medicine, 40(3), 239-246. https://doi.org/10.4103/ijpsym.ijpsym_561_17
Chaudhari, N., Dawalbhakta, M., & Nampoothiri, L. (2018). GnRH dysregulation in polycystic ovarian syndrome (PCOS) is a manifestation of an altered neurotransmitter profile. Reproductive Biology and Endocrinology, 16(1). https://doi.org/10.1186/s12958-018-0354-x
Cooney, L. G., & Dokras, A. (2017). Depression and Anxiety in Polycystic Ovary Syndrome: Etiology and Treatment. Curr Psychiatry Rep, 19(11), 83. https://doi.org/10.1007/s11920-017-0834-2
Coutinho, & Kauffman. (2019). The Role of the Brain in the Pathogenesis and Physiology of Polycystic Ovary Syndrome (PCOS). Medical Sciences, 7(8), 84. https://doi.org/10.3390/medsci7080084
Damone, A. L., Joham, A. E., Loxton, D., Earnest, A., Teede, H. J., & Moran, L. J. (2019). Depression, anxiety and perceived stress in women with and without PCOS: a community-based study. Psychol Med, 49(9), 1510-1520. https://doi.org/10.1017/s0033291718002076
Doretto, L., Mari, F. C., & Chaves, A. C. (2020). Polycystic Ovary Syndrome and Psychotic Disorder. Front Psychiatry, 11, 543. https://doi.org/10.3389/fpsyt.2020.00543
Enjezab, B., Eftekhar, M., & Ghadiri-Anari, A. (2017). Association between severity of depression and clinico-biochemical markers of polycystic ovary syndrome. Electronic Physician, 9(11), 5820-5825. https://doi.org/10.19082/5820
Esparza, L. A., Schafer, D., Ho, B. S., Thackray, V. G., & Kauffman, A. S. (2020). Hyperactive LH Pulses and Elevated Kisspeptin and NKB Gene Expression in the Arcuate Nucleus of a PCOS Mouse Model. Endocrinology, 161(4). https://doi.org/10.1210/endocr/bqaa018
Ethirajulu, A., Alkasabera, A., Onyali, C. B., Anim-Koranteng, C., Shah, H. E., Bhawnani, N., & Mostafa, J. A. (2021). Insulin Resistance, Hyperandrogenism, and Its Associated Symptoms Are the Precipitating Factors for Depression in Women With Polycystic Ovarian Syndrome. Cureus. https://doi.org/10.7759/cureus.18013
Gnawali, A., Patel, V., Cuello-Ramírez, A., Al Kaabi, A. S., Noor, A., Rashid, M. Y., . . . Mostafa, J. A. (2021). Why are Women With Polycystic Ovary Syndrome at Increased Risk of Depression? Exploring the Etiological Maze. Cureus. https://doi.org/10.7759/cureus.13489
Greenwood, E. A., Pasch, L. A., Cedars, M. I., Legro, R. S., Eisenberg, E., & Huddleston, H. G. (2018). Insulin resistance is associated with depression risk in polycystic ovary syndrome. Fertility and Sterility, 110(1), 27-34. https://doi.org/10.1016/j.fertnstert.2018.03.009
Greenwood, E. A., Yaffe, K., Wellons, M. F., Cedars, M. I., & Huddleston, H. G. (2019). Depression Over the Lifespan in a Population-Based Cohort of Women With Polycystic Ovary Syndrome: Longitudinal Analysis. The Journal of Clinical Endocrinology & Metabolism, 104(7), 2809-2819. https://doi.org/10.1210/jc.2019-00234
Hanson, B., Johnstone, E., Dorais, J., Silver, B., Peterson, C. M., & Hotaling, J. (2017). Female infertility, infertility-associated diagnoses, and comorbidities: a review. Journal of Assisted Reproduction and Genetics, 34(2), 167-177.
https://doi.org/10.1007/s10815-016-0836-8
He, F.-F., & Li, Y.-M. (2020). Role of gut microbiota in the development of insulin resistance and the mechanism underlying polycystic ovary syndrome: a review. Journal of Ovarian Research, 13(1). https://doi.org/10.1186/s13048-020-00670-3
Hung, J.-H., Hu, L.-Y., Tsai, S.-J., Yang, A. C., Huang, M.-W., Chen, P.-M., . . . Shen, C.-C. (2014). Risk of Psychiatric Disorders following Polycystic Ovary Syndrome: A Nationwide Population-Based Cohort Study. PLoS ONE, 9(5), e97041. https://doi.org/10.1371/journal.pone.0097041
Ilie, I. R. (2020). Neurotransmitter, neuropeptide and gut peptide profile in PCOS-pathways contributing to the pathophysiology, food intake and psychiatric manifestations of PCOS. Adv Clin Chem, 96, 85-135. https://doi.org/10.1016/bs.acc.2019.11.004
Jamilian, M., Mansury, S., Bahmani, F., Heidar, Z., Amirani, E., & Asemi, Z. (2018). The effects of probiotic and selenium co-supplementation on parameters of mental health, hormonal profiles, and biomarkers of inflammation and oxidative stress in women with polycystic ovary syndrome. Journal of Ovarian Research, 11(1). https://doi.org/10.1186/s13048-018-0457-1
Katulski, K., Podfigurna, A., Czyzyk, A., Meczekalski, B., & Genazzani, A. D. (2018). Kisspeptin and LH pulsatile temporal coupling in PCOS patients. Endocrine, 61(1), 149-157. https://doi.org/10.1007/s12020-018-1609-1
Liang, Z., Di, N., Li, L., & Yang, D. (2021). Gut microbiota alterations reveal potential gut-brain axis changes in polycystic ovary syndrome. J Endocrinol Invest, 44(8), 1727-1737. https://doi.org/10.1007/s40618-020-01481-5
Moore, A. M., & Campbell, R. E. (2017). Polycystic ovary syndrome: Understanding the role of the brain. Front Neuroendocrinol, 46, 1-14. https://doi.org/10.1016/j.yfrne.2017.05.002
Ostad Mohammadi, V., Jamilian, M., Bahmani, F., & Asemi, Z. (2019). Vitamin D and probiotic co-supplementation affects mental health, hormonal, inflammatory and oxidative stress parameters in women with polycystic ovary syndrome. Journal of Ovarian Research, 12(1). https://doi.org/10.1186/s13048-019-0480-x
Qadri, S., Hussain, A., Bhat, M. H., & Baba, A. A. (2018). Polycystic Ovary Syndrome in Bipolar Affective Disorder: A Hospital-based Study. Indian Journal of Psychological Medicine, 40(2), 121-128. https://doi.org/10.4103/ijpsym.ijpsym_284_17
Qi, J., Wang, W., Zhu, Q., He, Y., Lu, Y., Wang, Y., . . . Sun, Y. (2018). Local Cortisol Elevation Contributes to Endometrial Insulin Resistance in Polycystic Ovary Syndrome. The Journal of Clinical Endocrinology & Metabolism, 103(7), 2457-2467. https://doi.org/10.1210/jc.2017-02459
Rees, D. A., Udiawar, M., Berlot, R., Jones, D. K., & O'Sullivan, M. J. (2016). White Matter Microstructure and Cognitive Function in Young Women With Polycystic Ovary Syndrome. The Journal of Clinical Endocrinology & Metabolism, 101(1), 314-323. https://doi.org/10.1210/jc.2015-2318
Remes, O., Brayne, C., Van Der Linde, R., & Lafortune, L. (2016). A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain and Behavior, 6(7), e00497. https://doi.org/10.1002/brb3.497
ROC Curve in Evaluation of Diagnostic Value of Serum 25-hydroxyvitamin-D for PCOS with Depression. (2020). Journal of the College of Physicians and Surgeons Pakistan, 30(06), 659-661. https://doi.org/10.29271/jcpsp.2020.06.659
Rodriguez-Paris, D., Remlinger-Molenda, A., Kurzawa, R., Głowińska, A., Spaczyński, R., Rybakowski, F., . . . Banaszewska, B. (2019). Psychiatric disorders in women with polycystic ovary syndrome. Psychiatr Pol, 53(4), 955-966. https://doi.org/10.12740/PP/OnlineFirst/93105 (Występowanie zaburzeń psychicznych u kobiet z zespołem policystycznych jajników.)
Sirmans, S., & Pate, K. (2013). Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clinical Epidemiology, 1. https://doi.org/10.2147/clep.s37559
Szeliga, A., Rudnicka, E., Maciejewska-Jeske, M., Kucharski, M., Kostrzak, A., Hajbos, M., . . . Meczekalski, B. (2022). Neuroendocrine Determinants of Polycystic Ovary Syndrome. International Journal of Environmental Research and Public Health, 19(5), 3089. https://doi.org/10.3390/ijerph19053089
Teede, H., Deeks, A., & Moran, L. (2010). Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Medicine, 8(1), 41.
https://doi.org/10.1186/1741-7015-8-41
Witchel, S. F., Oberfield, S. E., & Peña, A. S. (2019). Polycystic Ovary Syndrome: Pathophysiology, Presentation, and Treatment With Emphasis on Adolescent Girls. Journal of the Endocrine Society, 3(8), 1545-1573. https://doi.org/10.1210/js.2019-00078
Sapolsky, R. M. (2018). Behave: The biology of humans at our best and worst. Penguin Press.
Downloads
Posted
Versions
- 2022-12-24 (3)
- 2022-12-24 (2)
- 2022-11-01 (1)
Categories
License
Copyright (c) 2022 Karis Sarkisian

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.

